ARTICLE. Bajo Peña L, Espaulella Panicot J, Dalmau Paniagua N, Barneto Soto M, Altimiras Roset J. Rev Esp Geriatr Gerontol. 2013;48(2):69-71.
Abstract.
Aim: To determine the characteristics of patients with dementia who died in a psychogeriatric unit, and to describe the conditions that led to their death.
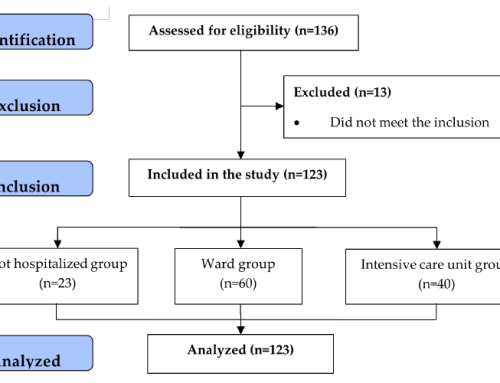
Materials and Methods: Observational study of patients who died in the Psychogeriatric unit of Hospital de la Santa Creu de Vic during a three and a half year period.
Results: Of the 554 patients admitted during the study period, we recorded a mortality of 14.6% (81 patients). The analysis of those who died showed that 67.9% were women, with a mean age of 85.8 years, with the most frequent cause being Alzheimer type dementia (37%) and being in an advanced stage (CDR3, GDS 6-7) in 72.8% of cases. On admission the following characteristics were recorded: Mini Mental State Examination (MMSE) 9.5, Barthel Index (BI) prior to entry 50.1, BI on admission 17.4, and Neuropsychiatric Inventory (NPI) 31.4. A therapeutic limitation treatment was determined for 84% of patients on admission. From the analysis of the conditions that lead to death it was noted that: In 74.1% of the patients the death was a direct result of a triggering event (the most frequent being respiratory infection), in 17.3% the death occurred by a gradual decline, with no clear precipitating factor, and in 8.6% of patients palliative sedation was required due to poorly controlled symptoms.
Conclusions: Intercurrent problems were the most common factors related to the death of the patients. Most patients died in the stages prior to the established criteria for terminal dementia. In some cases patients may experience disorder behavior as a refractory symptom.







Leave a Reply