Abstract
Background-Chronic wounds are a worldwide problem. One advanced biological therapy is platelet-rich plasma (PRP). Many studies have demonstrated the efcacy of PRP therapy in chronic wounds of diferent etiologies, but results are not conclusive.
Objective- This systematic review intends to identify high-level clinical trials or randomized controlled trials (RCTs) that compare autologous platelet-rich plasma with alternative treatments for chronic cutaneous wounds in humans. Moreover, it investigates whether patients who have received autologous PRP therapy for chronic wound care for diverse etiologies have a better clinical outcome than patients treated with alternative treatments.
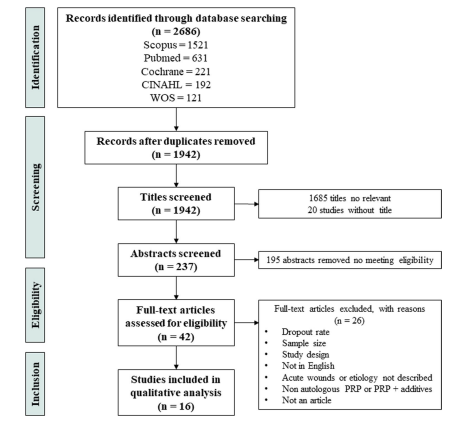
Methods- PubMed, Scopus, Web of Science (WOS), The Cochrane Library, and Cumulative Index of Nursing and Allied Literature Complete (CINAHL) were searched in May 2021. The search was performed without any restriction. The studies were selected and reviewed by two authors on the basis of predefned inclusion criteria and following PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analyses) guidelines, and a third author was consulted in the event of disagreement. All of the studies included were assessed using the Study Quality Assessment Tool for Controlled Intervention Studies published by the National Heart, Lung, and Blood Institute (NIH, USA).
Results- Of the 2686 studies identifed in the search, 16 RCTs met the inclusion criteria. Of the studies included, nine deal with diabetic wounds, fve with venous wounds, one with arterial wounds, and one with pressure wounds. The studies included showed diferent PRP obtention and application methods due to a lack of standardized clinical guidelines. All studies dealing with venous ulcers showed an increase in wound healing among patients treated with PRP compared with the control group. Diabetic wound trials are non-conclusive due to the heterogeneity of the reported results. Only one study of arterial and one of pressure ulcers were identifed, so no comparison can be made. Most of the articles included in the study had an unclear or low risk of bias, except in sample size power calculation.
Conclusions- PRP may improve the healing of venous ulcers; however, there is no strong evidence regarding this positive efect in other wound etiologies. Although autologous PRP therapy is widely used, its efectiveness according to wound etiology is still not clear. The heterogenicity of the protocols to prepare and apply PRP therapy and the diferent methods for measuring chronic wound outcomes hinder the comparison of studies, thereby limiting the possibility of conducting a more robust analysis.







Leave A Comment