Authors: Oriol Aguiló, Joan Carles Trullàs, Begoña Espinosa, Pedro López-Ayala, Víctor Gil,10 María Luisa López-Grima, Pablo Herrero-Puente, Javier Jacob, María Pilar López-Díez, José Manuel Garrido, Javier Millán, Alfonso Aguirre, Pascual Piñera, Christian E. Müller, Pere Llorens, Òscar Miro.
Abstract
Objective: To determine the prevalence, characteristics, timing of implementation and prognosis of patients with left bundle branch block (LBBB) and acute heart failure (AHF) treated with cardiac resynchronization therapy (CRT) in a real-life registry.
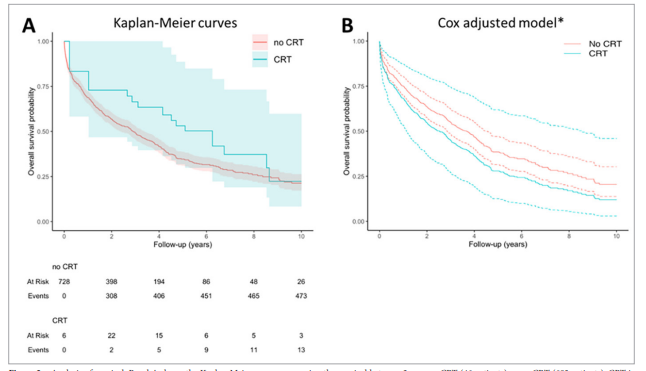
Methods: We analysed the characteristics of patients with AHF and LBBB at the time of inclusion in the EAHFE (Epidemiology Acute Heart Failure Emergency) cohort to determine the indication for CRT, the timing of implementation and its impact on 10-year all-cause mortality.
Results: 729 patients with a median age of 82 years and there was a high burden of comorbidities and functional dependence. The median left-ventricle ejection fraction (LVEF) was 40%. Forty-six (6%) patients were treated with CRT at some point during follow-up, with a median time of delay for CRT implementation of 960 (IQR=1147 days) and at least 108 more untreated patients fulfilled criteria for CRT. Patients receiving CRT were younger, had different comorbidities, less functional dependence (higher Barthel index) and lower LVEF values. The median follow-up was 5.7 years (95% CI: 5.6-5.8) and CRT was not associated with changes in 10-year mortality (adjusted HR 1.33, 95% CI: 0.72-2.48; p-value 0.4). When compared with untreated patients fulfilling criteria for CRT, very similar results were observed (adjusted HR 1.34, 95% CI: 0.67-2.68).
Conclusions: CRT implementation was delayed and underused in patients with AHF and LBBB. Under these circumstances, CRT is not associated with a reduction in all-cause mortality in the long term.









Leave a Reply